Blood Transfusion: A Comprehensive Guide
Blood transfusion is a medical procedure in which donated blood or blood components are transferred into a recipient’s bloodstream. It is a critical procedure for treating various conditions, including severe blood loss, anaemia, and certain medical disorders like hypovolemic shock, thalassemia & RTA cases.
Objectives of Blood Transfusion:
- Replace lost blood due to surgery, injury, or trauma.
- Treat conditions like severe anaemia or haemoglobin disorders.
- Support patients undergoing chemotherapy or bone marrow transplants.
- Correct clotting deficiencies or platelet disorders.
Components of Blood for Transfusion:
- Whole Blood: Contains red blood cells, white blood cells, platelets, and plasma. Rarely used today.
- Red Blood Cells (Packed RBCs): Used to treat anaemia and significant blood loss.
- Platelets: Help in clotting; used for conditions like thrombocytopenia.
- Plasma: Contains clotting factors and proteins; used in clotting disorders & plasmapheresis.
- Cryoprecipitate: Rich in fibrinogen, used for specific clotting deficiencies.
Indications for Blood Transfusion:
- Acute Blood Loss: Due to trauma, surgery, or childbirth.
- Anaemia: When the haemoglobin level is critically low.
- Bleeding Disorders: Such as hemophilia or von Willebrand disease.
- Cancer Treatment: To replenish blood cells reduced during chemotherapy.
- Chronic Illnesses: Conditions like sickle cell anaemia or thalassemia.
Procedure Steps for Blood Transfusion:
- Preparation:
- Doctor’s Order: Ensure the transfusion is medically necessary.
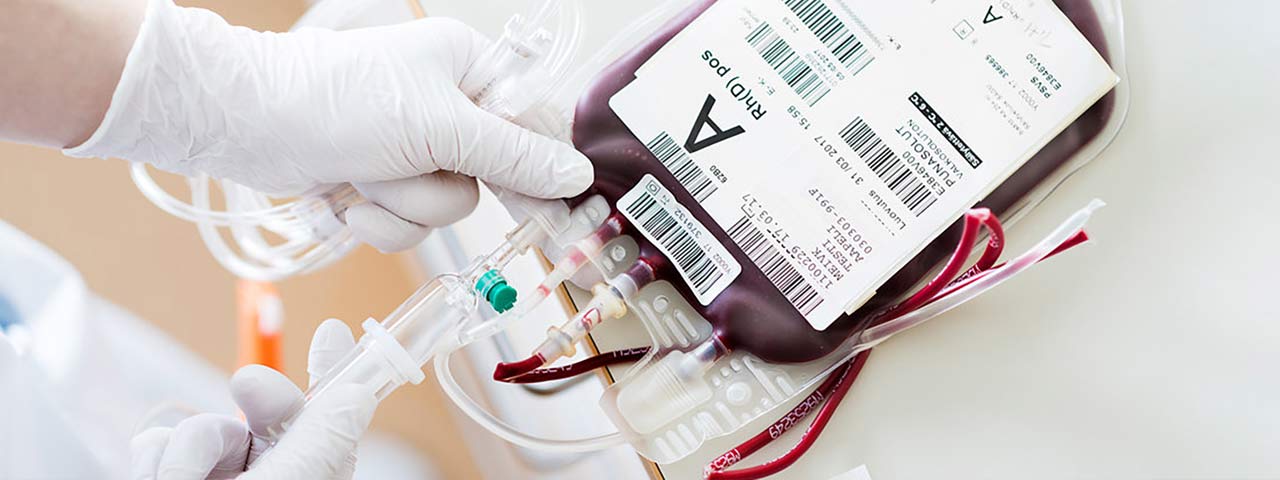
- Blood Typing and Cross-Matching:
- Confirm the patient’s blood type and match it with the donor’s blood.
- Perform a cross-match test to ensure compatibility and prevent reactions.
- Informed Consent: Explain the procedure, risks, and benefits to the patient and obtain consent.
- Equipment Required:
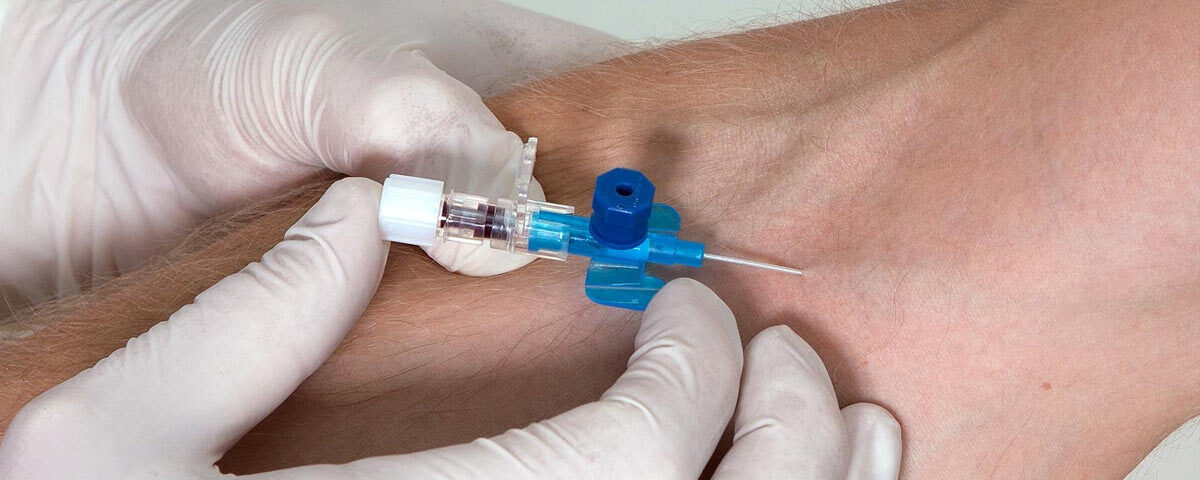
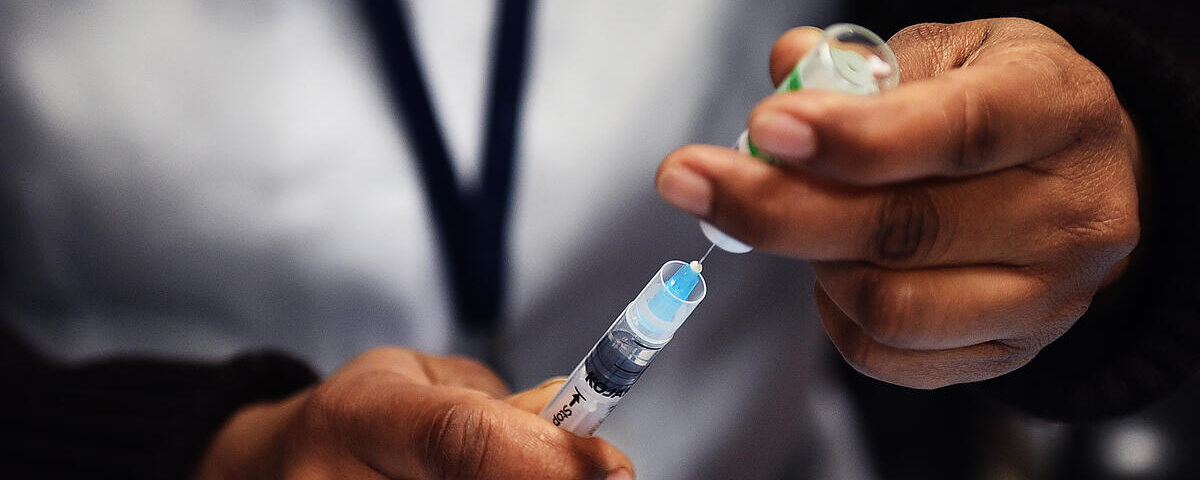
- IV cannula and BT set with a blood filter.
- Blood product (stored at appropriate temperature).
- Normal saline (to flush the IV line).
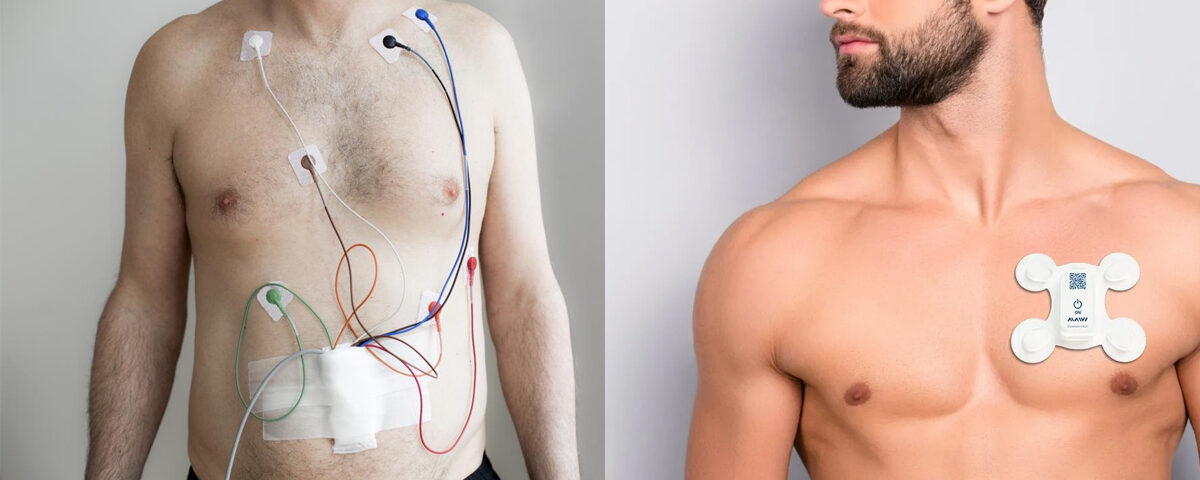
- Monitoring equipment (blood pressure cuff, thermometer).
- Emergency drugs and equipment for managing transfusion reactions.
- Starting the Transfusion:
- Check the Blood Bag:
- Verify the label for blood type, expiration date, and volume.
- Inspect the bag for clots, discolouration, or leaks.
- Prepare the IV Line:
- Insert an IV cannula into the patient’s vein.
- Prime the tubing with saline to prevent blood clotting in the line.
- Begin Transfusion:
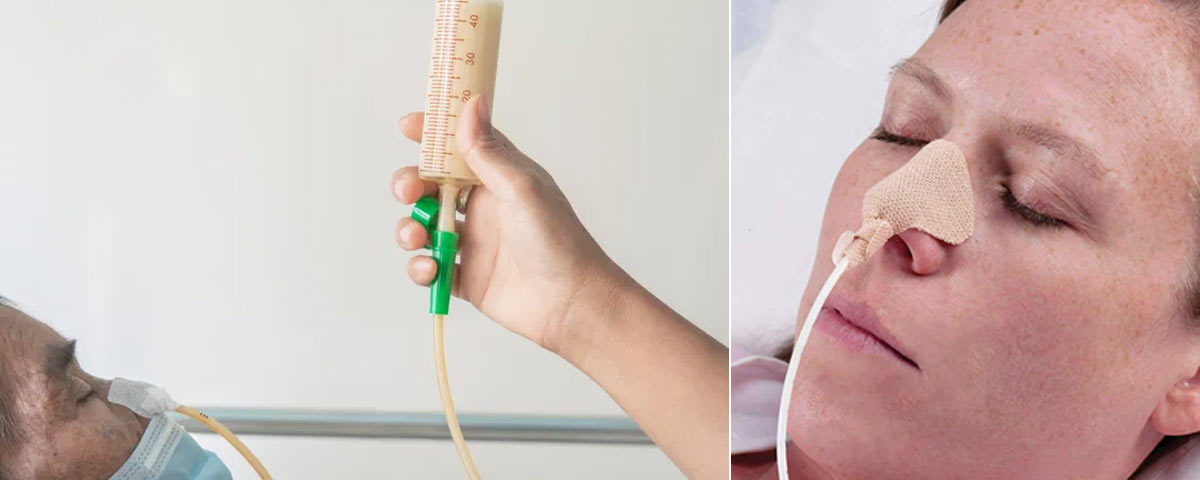
- Start at a slow rate (e.g., 2 mL/min) to monitor for immediate reactions.
- Check for vitals including temperature, heart rate and BP.
- After 15 minutes, if no reaction occurs, increase to the prescribed rate.
- Monitoring During Transfusion:
- Check vital signs (temperature, blood pressure, heart rate) in every 15 minutes initially, then periodically.
- Observe the patient for symptoms of adverse reactions (see below).
- After the Transfusion:
- Flush the IV line with saline.
- Document the procedure, including the type of blood product, start and end times, and patient’s response.
- Dispose of used materials as per medical waste protocols.
Signs of Transfusion Reactions:
Reactions are rare but can be life-threatening. Monitor the patient closely for:
- Fever or Chills: Indicates febrile reaction or infection.
- Shortness of Breath or Chest Pain: May indicate a hemolytic reaction or fluid overload which may lead to heart failure.
- Rash or Itching: Suggests an allergic reaction.
- Back Pain or Dark Urine: Signs of haemolysis (destruction of red blood cells).
- Drop in Blood Pressure: Possible anaphylaxis which may lead to anaphylactic shock or septic shock.
What to Do in Case of a Reaction:
- Stop the transfusion immediately.
- Keep the IV line open with saline.
- Notify the healthcare provider and follow emergency protocols.
- Administer medications (e.g., antihistamines, corticosteroids, epinephrine) as prescribed.
- Return the blood bag and tubing to the blood bank for investigation.
Post-Transfusion Care:
- Monitor the patient for delayed reactions (e.g., jaundice or fever) for 24–48 hours.
- Encourage the patient to report symptoms like fatigue, dark urine, or persistent fever.
- Check haemoglobin levels to ensure the transfusion achieved its purpose.
Risks of Blood Transfusion:
- Infections: Extremely rare due to stringent blood screening.
- Iron Overload: With multiple transfusions.
- Allergic Reactions: Hives, itching, or fever.
- Haemolytic Reaction: Occurs when there is a mismatch between donor and recipient blood.
- Fluid Overload: Especially in elderly or cardiac patients.
Would you like more detailed information about blood products, managing specific complications, or patient education for blood transfusions?